Department Introduction
Internal Medicine | Our Speciality
:::

Our Speciality
Chest Pain Center(Cardiovascular Unit)
To provide timely medical services for acute critically cardiovascular emergency patients, we established the first chest pain center in Taiwan in July 2009. We have attending physicians specializing in cardiovascular provide shifts in 24/7 coverage and the comprehensive medical care at the first moment. In addition to offering the emergent cardiac catheterization at the first moment, we also introduce, if necessary, intra-aortic balloon pump (IABP), extracorporeal membrane oxygenation (ECMO) and therapeutic hypothermia to save patients’ lives and prevent complications. We achieve a rapid door-to-balloon time (D2B, the amount of time between a heart attack patient's arrival at the hospital to the time he/she receives percutaneous coronary intervention) of <55 minutes, which is far shorter than the international goal, no more than 90 minutes. The patients’ survivor rate of ST segment elevation myocardial infarction is more than 95%. We won the Symbol of National Quality by Institution of Biotechnology and Medicine Industry (IBMI) and the Coronary Syndrome Disease Care Certification by Joint Commission of Taiwan, and became a reliable referral center for acute critically cardiovascular emergency patients in central area of Taiwan.

Interventional Bronchoscopy Center (Division of Chest Medicine)
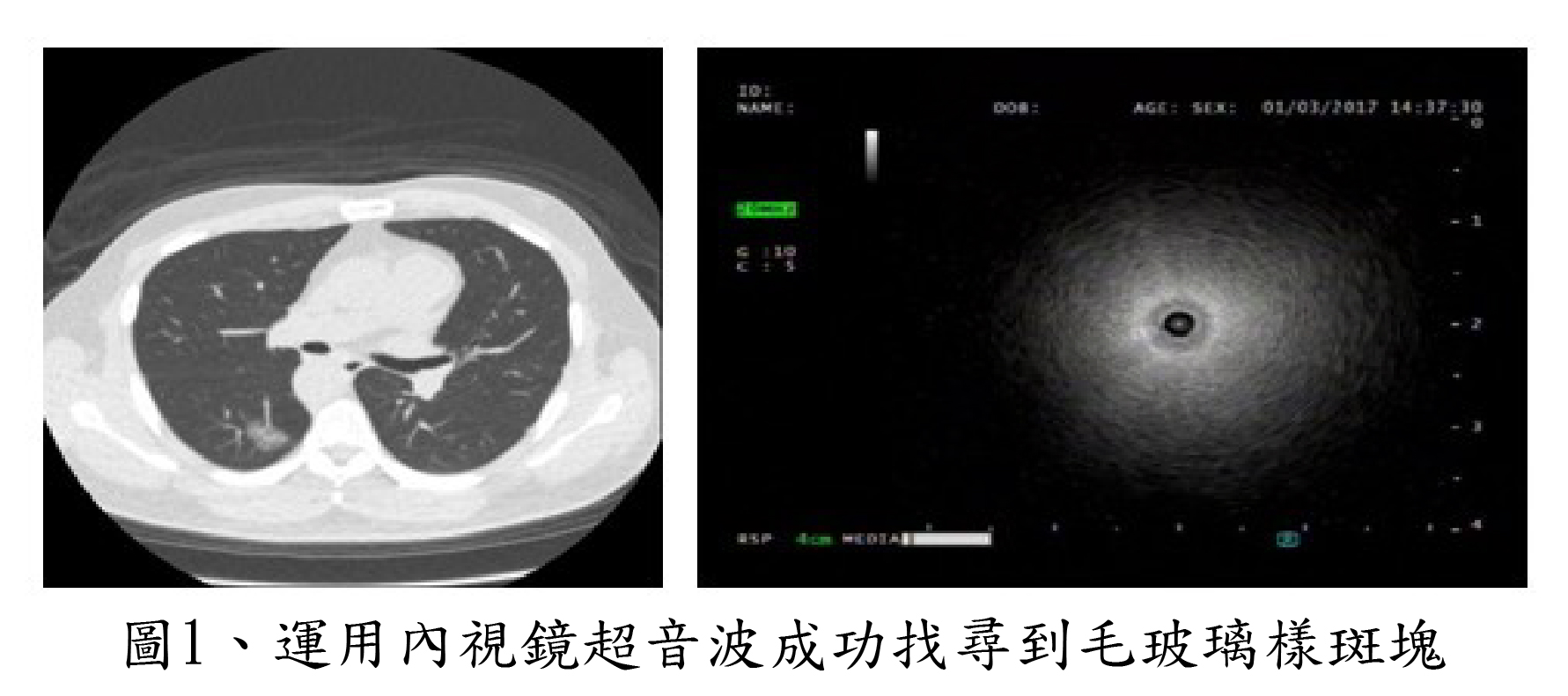
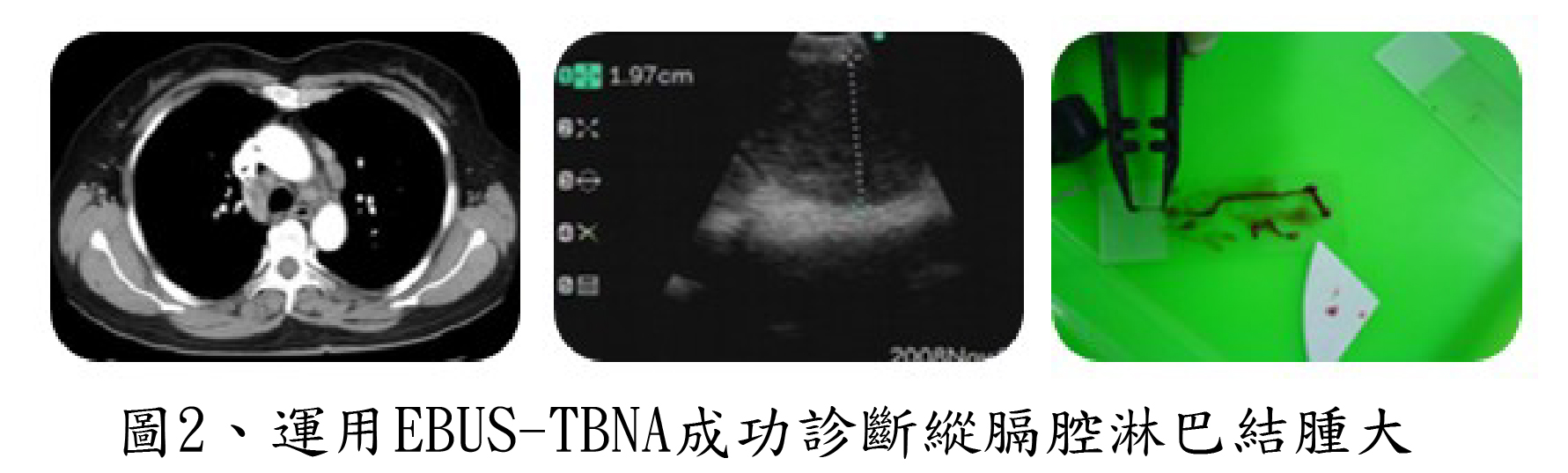
The division of chest medicine of CMUH introduced bronchoscopic electrocautery and tracheobronchial stent placement in 2005, autofluorescence endoscopy in 2006, bronchoscopy-guided tracheostomy in 2007, and endobronchial ultrasound and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) in 2008. The interventional bronchoscopy ccenter has been established since then. The care team for both the diagnostic and therapeutic use of a bronchoscope is formed in order to provide comprehensive techniques and facilities to diagnose pulmonary diseases, detect the bronchial wall and mediastinal invasion by lung cancer, assess the extent of tumors in hilar pulmonary vasculature and offer a safe and efficient tracheotomy. Besides the cooperation within the care team, the standard operating procedure of implementing a bronchoscopy has been created to provide comprehensive medical care. We won the Symbol of National Quality by Institution of Biotechnology and Medicine Industry (IBMI), the first interventional bronchoscopy center winner in Taiwan.
The characteristics of the interventional bronchoscopy center are divided to two aspects
-
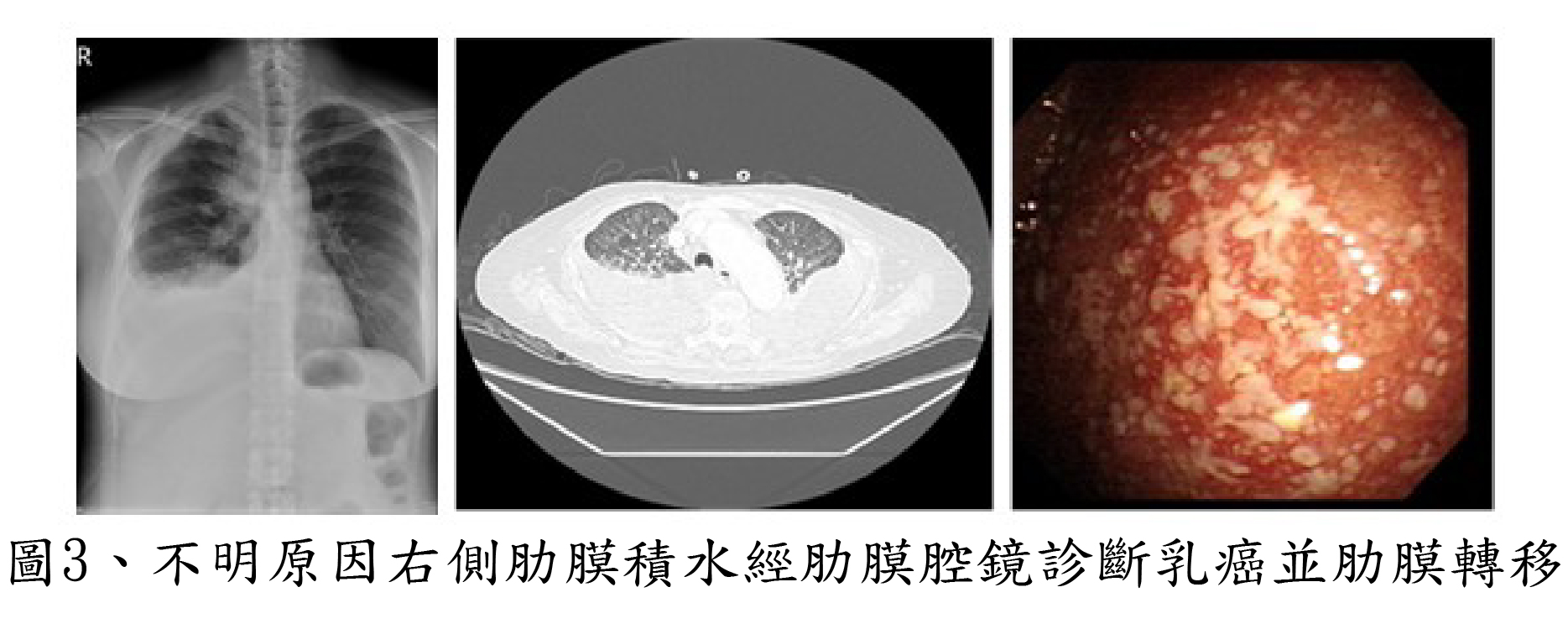
diagnostic and therapeutic: Diagnostic aspect: endobronchial ultrasound (EBUS, Figure 1.), endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA, Figure 2.) and medical thoracoscopy (Figure 3.)
-
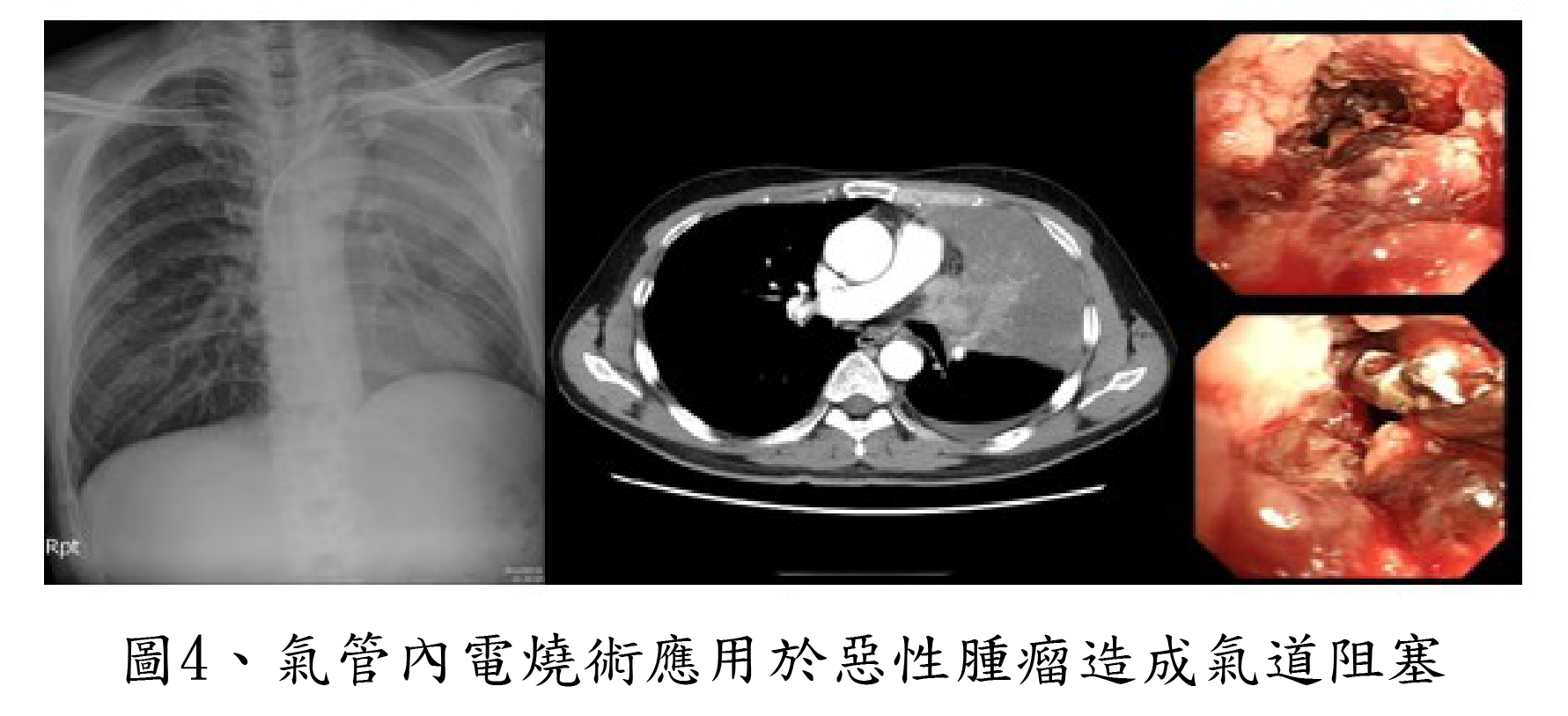
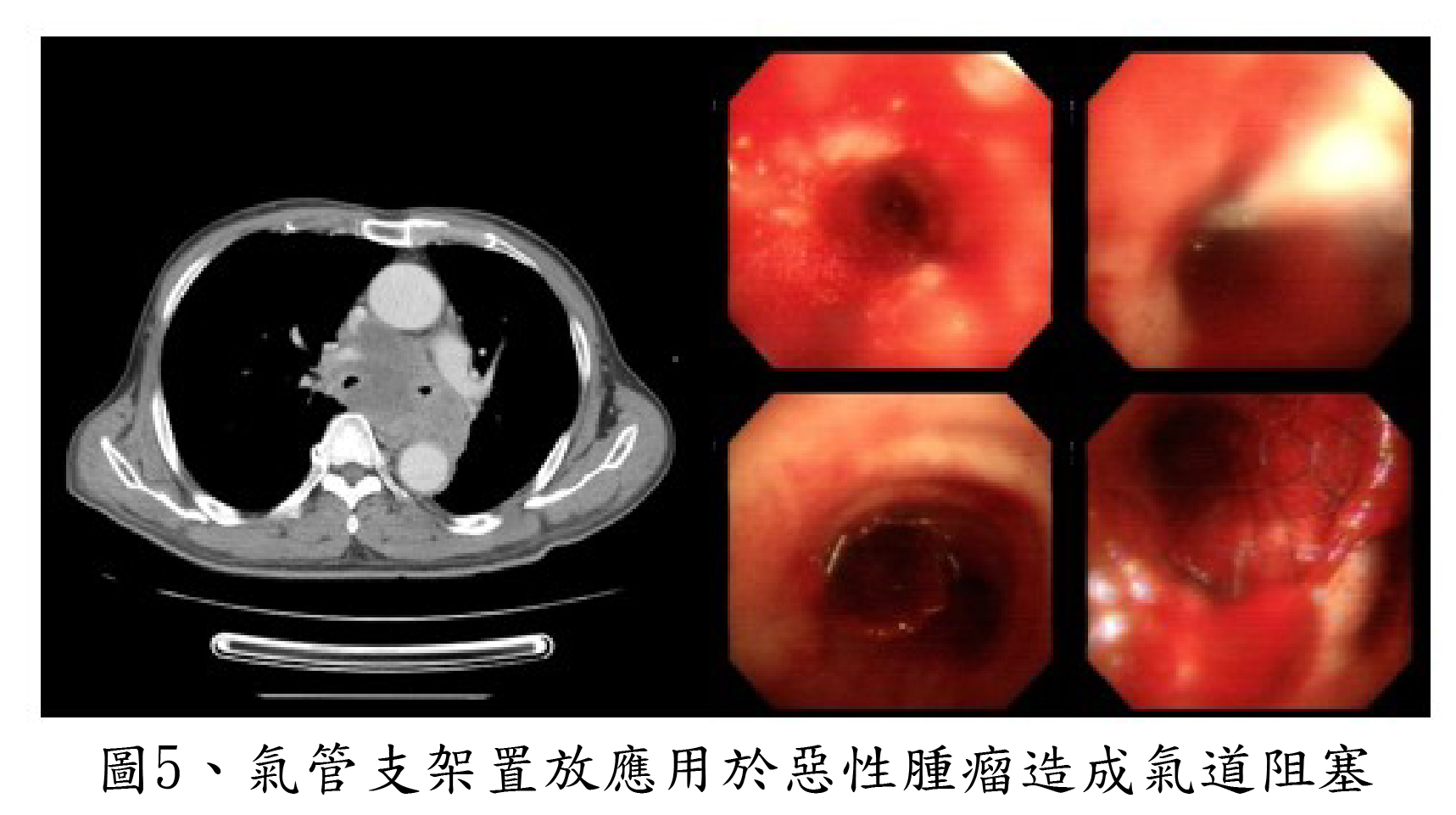
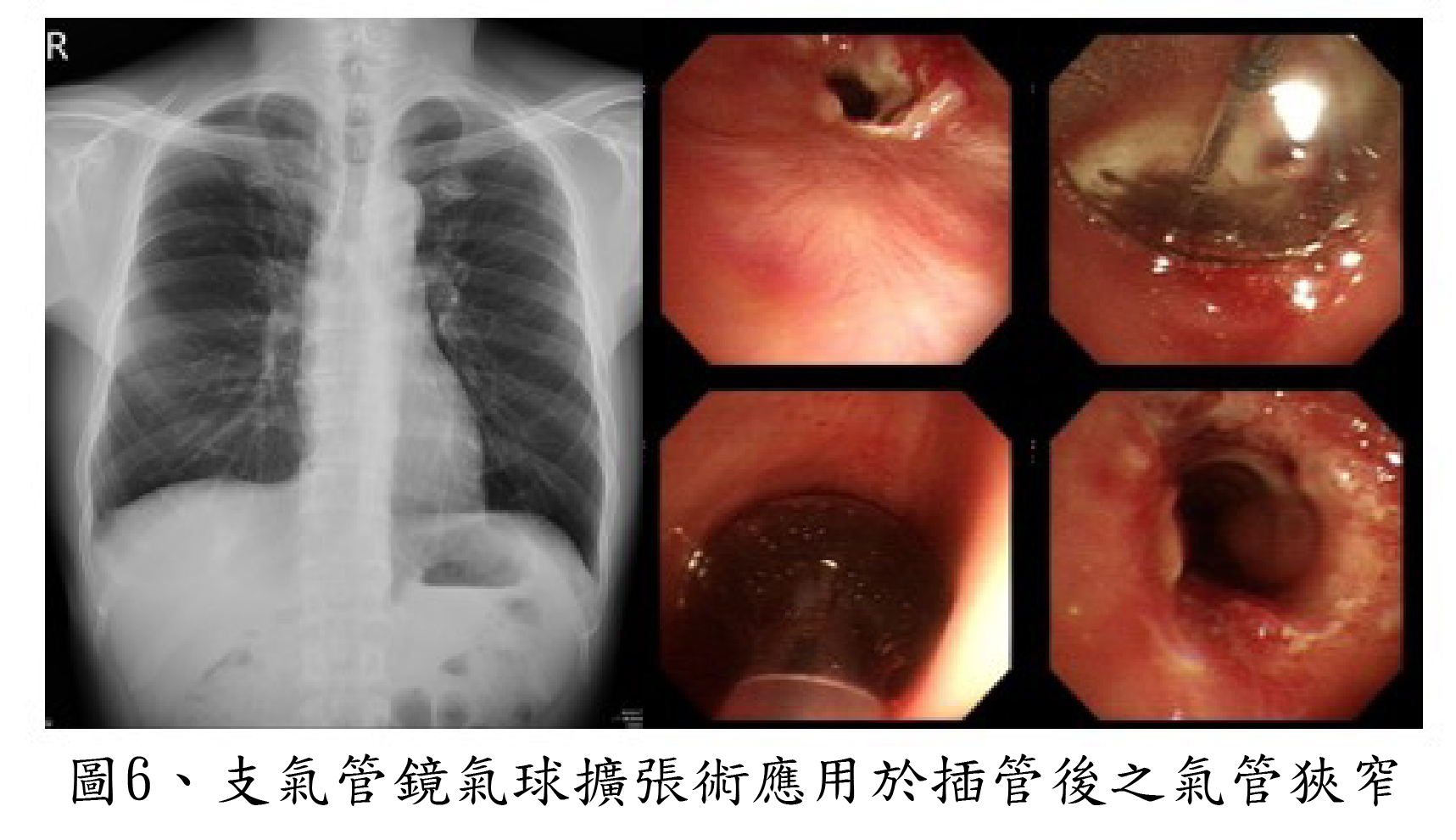
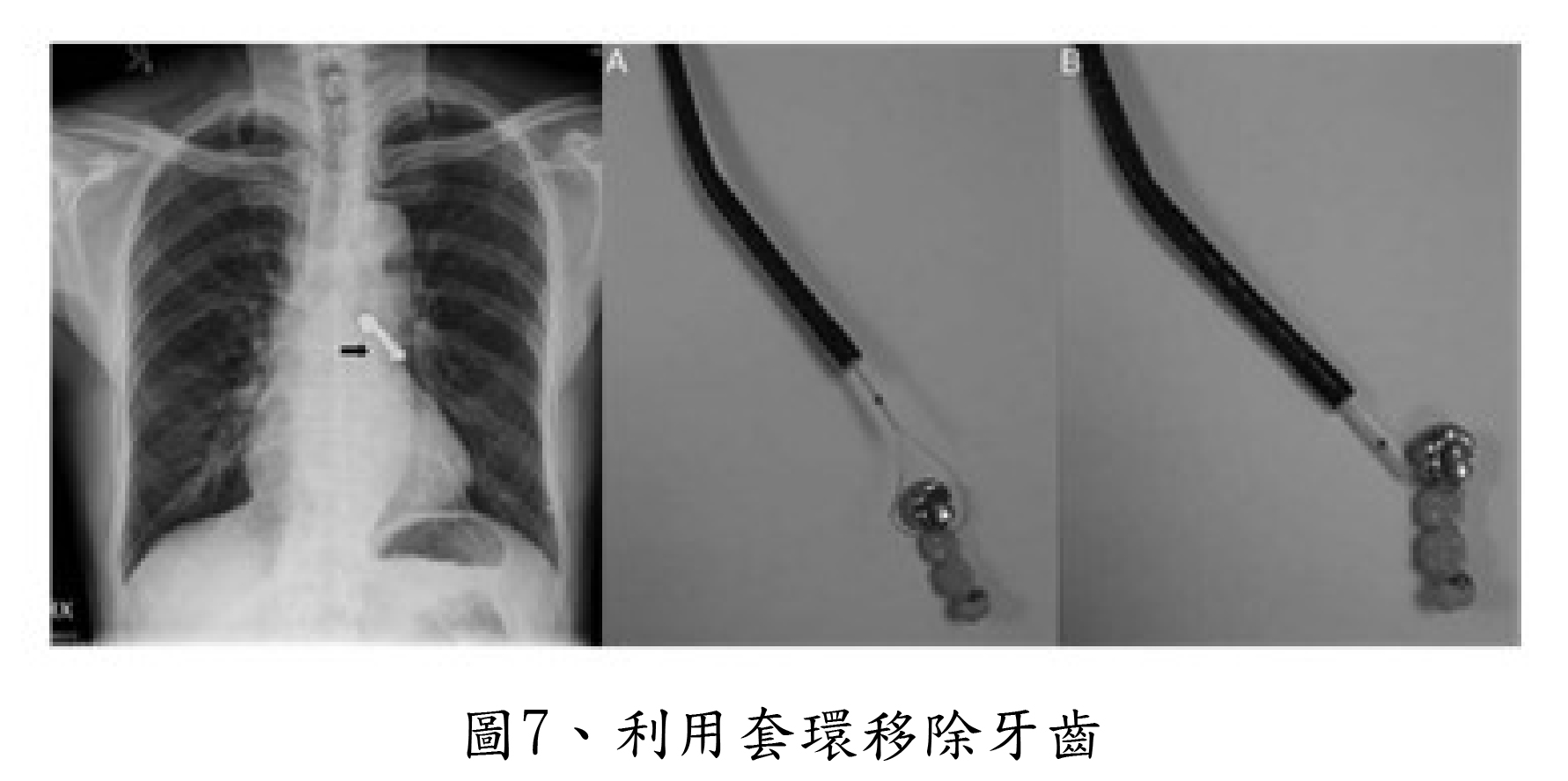
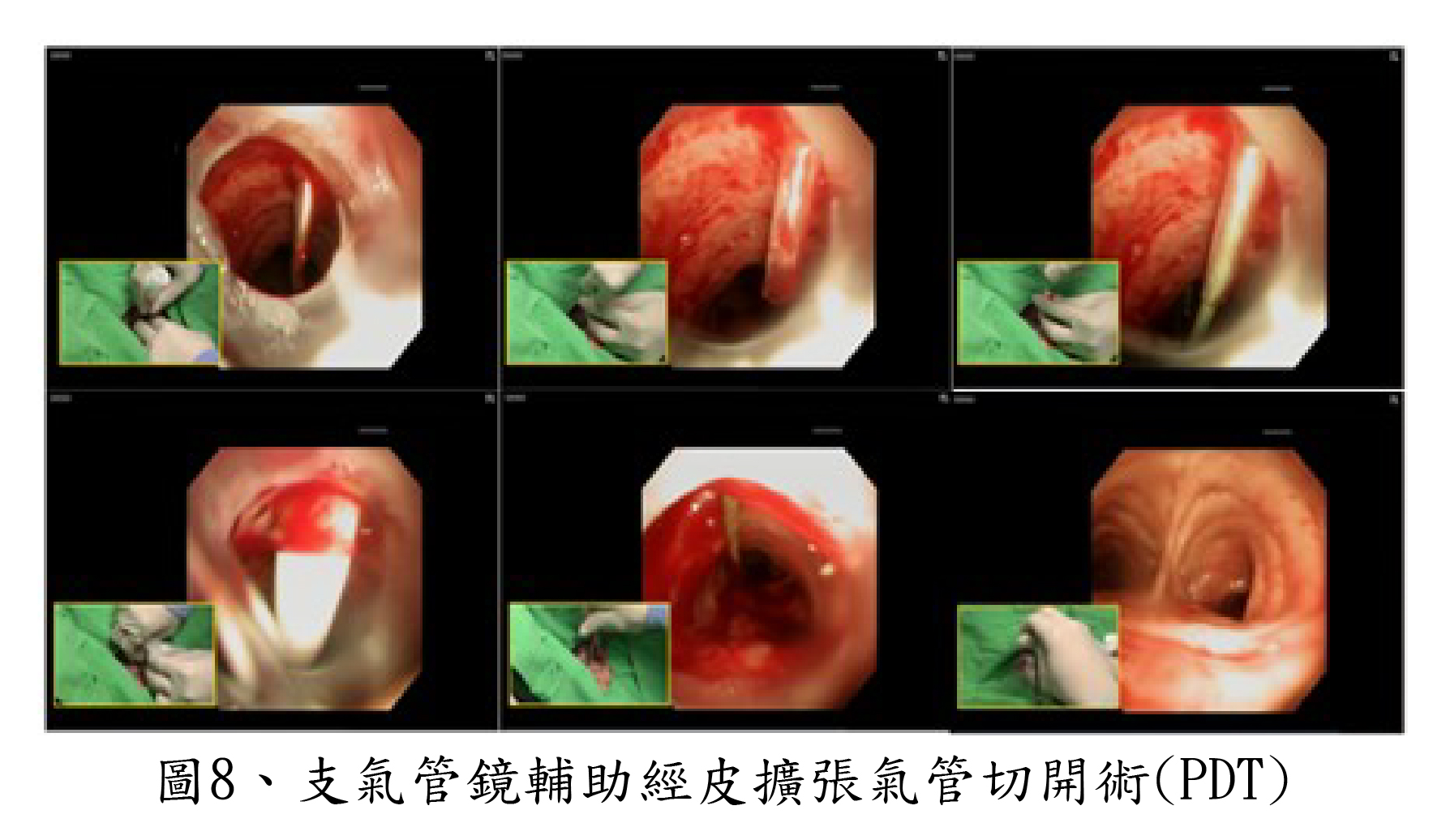
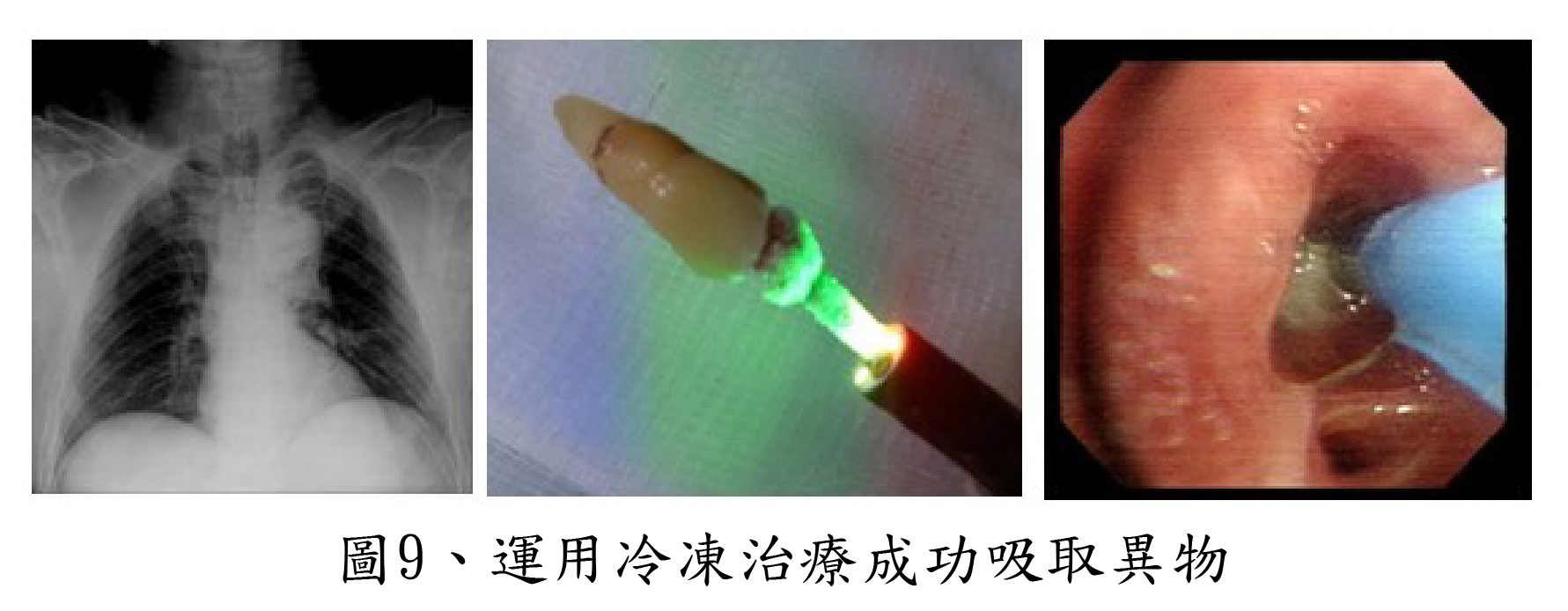
Therapeutic aspect: electrocoagulation (Figure 4.), tracheobronchial stent placement (Figure 5.), bronchoscopic balloon dilatation (Figure 6.), tracheal foreign body removal (Figure 7.), bronchoscopy-guided percutaneous dilational tracheostomy (Figure 8.), argon plasma coagulation (APC).
Endoscopic submucosal dissection, ESD (gastroenterology unit)
Implementing endoscopic submucosal dissection (ESD) is the reason why we stand out from all the medical centers in the field of therapeutic endoscopy.
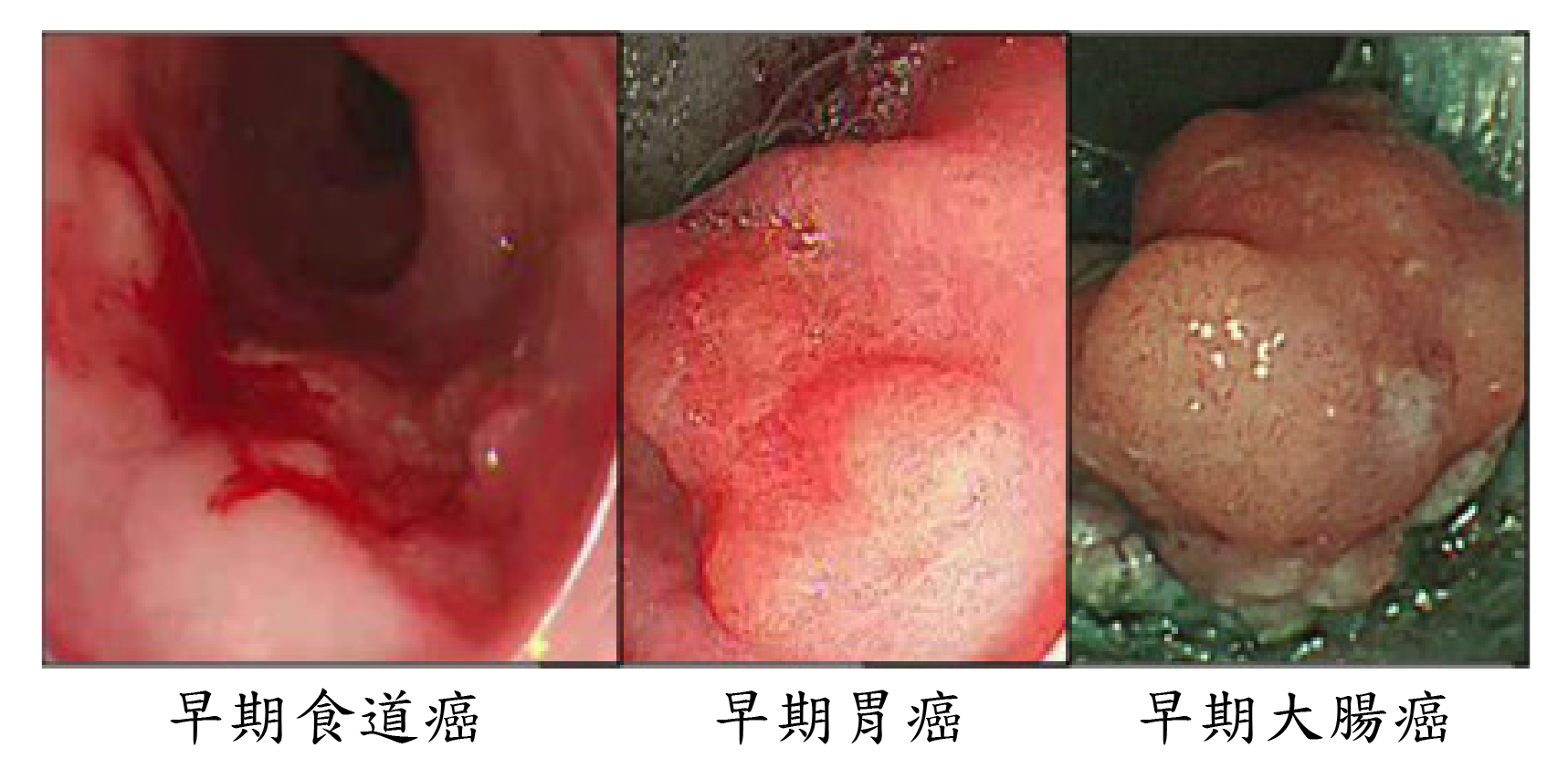
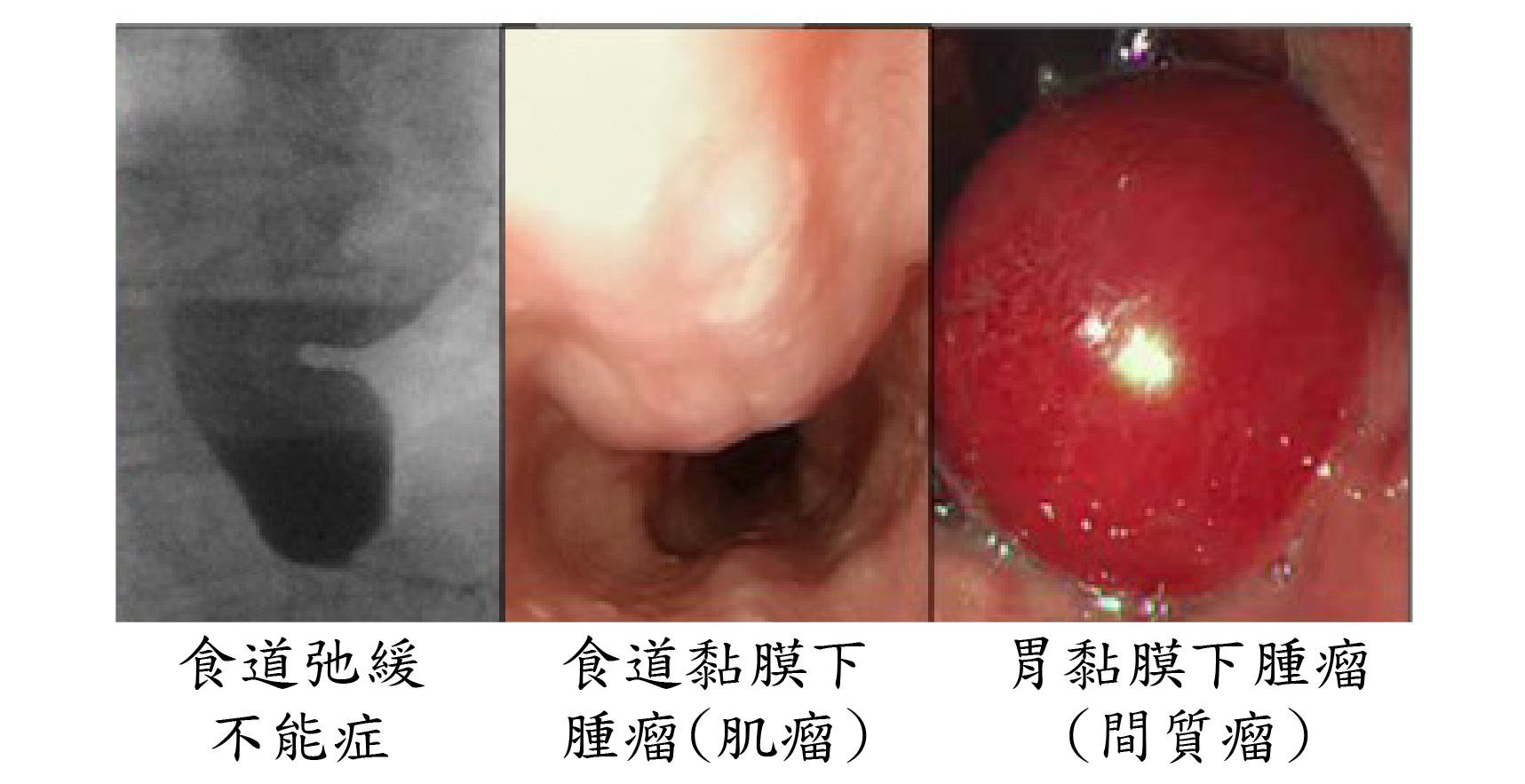
The indications of implementing ESD to remove gastrointestinal tumors include early-stage esophageal cancer, early-stage stomach cancer, early-stage colorectal cancer, flat adenoma of the colon and Barrett's esophagus. In addition, different kinds of gastric submucosal tumors, such as stromal tumor, neuroendocrine tumor, carcinoid, ectopic pancreas and lipoma, can be treated by ESD as well. Moreover, the patients with achalasia can be radically treated by per-oral endoscopic myotomy (POEM).
Among all clinical applications of ESD, the implementation on early-stage gastrointestinal malignant tumors has the most significant effect. This approach is feasible when the tumor is limited to mucosa or superficial submucosa without invasion or migration.
The applications of ESD include the following:
- Radical treatments of early-stage gastrointestinal malignant tumors and precancerous lesion: early-stage esophageal cancer, early-stage stomach cancer, early-stage colorectal cancer, high-grade gastric dysplasia, flat gastric polyps, flat adenoma of the colon and Barrett's esophagus.
- ESD as a radical treatment: stromal tumor, neuroendocrine tumor, carcinoid, ectopic pancreas and lipoma.
- Endoscopic treatment of achalasia (per-oral endoscopic myotomy, POEM)
Home Hemodialysis ( division of nephrology)
Chronic renal failure is a severe disease, the patients of which will end their lives if not accept kidney transplantation or hemodialysis. Due to unpopularity of organ donation in Taiwan, most patients can only continue their lives by hemodialysis. However, the survivor rate of patients on hemodialysis is not high; the five-year survival rate of patients on traditional hemodialysis is around 40% according to USRDS statistics. High flux membrane, hemodiafiltration and ultrapure water were all expected to improve survival rates but they never came true.
According to references from Tassin in France, patients treated with long dialysis sessions had significantly higher survival rate and quality of life. Therefore, home hemodialysis drew public’s attention. More and more developed countries started implementing home hemodialysis such as United Kingdom, Germany, Denmark, Netherland, Australia, New Zealand, United State and Canada. Hong Kong started in 2006 and got immense response from patients. Korea and China started pilot projects in 2008 as well. To provide a better quality and a higher survival rate of hemodialysis for end-stage renal disease patients, the division of nephrology also proposed a pilot project of home hemodialysis, with the assistance of Dr. Chiu-Ching Huang (the former chairman of the Taiwan Society of Nephrology) , to prolong patients’ life and enhance their quality of life.
The home hemodialysis training is an 8-hour hemodialysis at hospital. The training is 8-12 times for 6-8 hours per session. The training takes up to 8 weeks and has 24 sessions divided to three times a week (Monday, Wednesday and Friday). After training, patients should pass the test including troubleshooting of hemodialysis machine, dealing with a power outage, troubleshooting of RO water system and dealing with sudden emergencies such as earthquakes and fire outbreaks. The patients passing the test can implement home hemodialysis.
Early outcome: seven patients accomplished their trainings and implemented home hemodialysis. We expect more patients to participate in this pilot project of home hemodialysis and to enjoy the outcome.
stem cell transplantation ( the division of hematology and oncology)
The division of hematology and oncology is enthusiastic about curing leukemia and other hematologic diseases by hematopoietic stem cell transplantation (HSCT). Hematopoietic stem cells have the ability to differentiate into white blood cells, red blood cells and platelets, and restore human hematopoietic system. Allogeneic transplant can reset the immune system to fight cancers. To cope with different situations and sources, we have already successfully implemented transplantations in elderly patients and haplo-identical hematopoietic stem cell transplantation as well.In addition, we have implemented transplantations in patients from both home and abroad. Moreover, we won the Symbol of National Quality in 2010 since we treated hematologic diseases with rich experience and techniques.
The important facilities and techniques are as follows:
- The laboratory which follows the Good Tissue Practice (GTP): the quality of cells is emphasized in a cell therapy and all the procedures including cell collection, separation, processing, storage and defrosting should follow high-standard GTP.
- The technique of cell separation and collection: utilizing CliniMACS Cell Separator System to elect specific cells for a specific treatment.
- Class 100 High Efficiency Particulate Air Filter (HEPA) which maintains positive room air pressure to protect isolation wards.
▲
